Estimate correlation between Aspergillus Spp. and Asthma Patients
Keywords:
Aspergillus Spp, Asthma PatientsAbstract
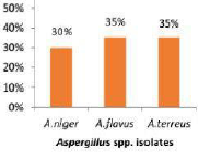
Fungal exposure is a daily fact of human existence that infrequently results in disease; Asthma is a chronic inflammatory disease of the airways characterized by respiratory symptoms such as wheeze, shortness of breath, chest tightness, and cough that vary over time and in intensity. The relationship between day-to-day changes in asthma severity and combined exposures to community air pollutants and aeroallergens remains to be clearly defined. There is a close association between fungi and asthma, the so-called fungal asthma. This study aimed to isolate the causative Aspergillus species that increase the risk of infection and to find out the association between asthma and Aspergillus spp. 40 sample of (sputum s and pharyngeal swabs) were collected from patients suffer from asthma symptoms. All samples were of both gender and of different age groups at the Specialized Center for Respiratory Diseases. Samples were grown on two culture media (SDA and MEA) and incubated at 37°C for 7 days. The numbers of positive samples were 32 on SDA medium, 29 on MEA medium. Isolates were identified using special culture media characteristics as well as macroscopic and microscopic analysis. Where A. flavus was found to be the most predominant species of the sputum (58%) and from the pharyngeal swab (58.82%) on SDA, while on MEA the most prominent species were A. flavus and A. terreus (35%) of the sputum and the pharyngeal swab was A.niger (42.11%). The Aspergillus genera showed resistance to Fluconazole, Amphotericin B and Nystatin. The study has concluded that, there is a correlation between asthma and Aspergillus species. Aspergillus flavus the most common Aspergillus associated with lung diseases (Asthma).
Downloads
References
Agarwal, R., Muthu, V., & Sehgal, I. S. (2023). Relationship between Aspergillus and asthma. AllergologyInternational, 72(4), 507-520.
Agbetile, J., Fairs, A., Desai, D., Hargadon, B., Bourne, M., Mutalithas, K., ... & Pashley, C.H. (2012).Isolation of filamentous fungi from sputum in asthma is associated with reduced post-bronchodilator FEV1.Clinical & Experimental Allergy, 42(5), 782-791
Alastruey-Izquierdo, A., Melhem, M.S., Bonfietti, L.X., & RodriguezTudela, J.L. (2015). Susceptibility testfor fungi: clinical and laboratorial correlations in medical mycology. Revista do Instituto de MedicinaTropical de São Paulo, 57, 57-64.
Badiee, P., & Hashemizadeh, Z. (2014). Opportunistic invasive fungal infections: diagnosis & clinicalmanagement. The Indian journal of medical research, 139(2), 195.
Bruce, D. L., Macartney, T., Yong, W., Shou, W., & Sapkota, G. P. (2012). Protein phosphatase 5 modulatesSMAD3 function in the transforming growth factor-ẞ pathway. Cellular signalling, 24(11), 1999-2006.
Busse, W., Corren, J., Lanier, B.Q., McAlary, M., Fowler-Taylor, A., Della Cioppa, G., & Gupta, N. (2001).Omalizumab, anti-IgE recombinant humanized monoclonal antibody, for the treatment of severe allergicasthma. Journal of allergy and clinical immunology, 108(2), 184-190.
Campo, P., Rodríguez, F., Sánchez-García, S., Barranco, P., Quirce, S., Pérez- Francés, C.,... & Delgado, J.(2013). Phenotypes and endotypes of uncontrolled severe asthma: new treatments. Journal of InvestigationAllergol Clinical Immunology, 23(2), 76-88.
Castro-Fuentes, C. A., Reyes-Montes, M. D. R., Frías-De-León, M. G., Valencia-Ledezma, O. E., Acosta-Altamirano, G., & Duarte-Escalante, E. (2022). Aspergillus-SARS-CoV-2 known?. Pathogens, 11(11), 1227.coinfection: what is
Chakrabarti, A., & Slavin, M. A. (2011). Endemic fungal infections in the Asia- Pacific region. MedicalMycology, 49(4), 337-344.
Chaverri, P., Branco-Rocha, F., Jaklitsch, W., Gazis, R., Degenkolb, T., & Samuels, G.J. (2015). Systematicsof the Trichoderma harzianum species complex and the re-identification of commercial biocontrol strains.Mycologia, 107(3), 558-590.
Daly, P., & Kavanagh, K. (2001). Pulmonary aspergillosis: clinical presentation,diagnosis and therapy. Britishjournal of biomedical science, 58(3), 197-205.
Denis, J., Forouzanfar, F., Herbrecht, R., Toussaint, E., Kessler, R., Sabou, M., & Letsher-Bru, V. (2018).Evaluation of two commercial real-time PCR kits for Aspergillus DNA detection in bronchoalveolar lavagefluid in patients with invasive pulmonary aspergillosis. The Journal of Molecular Diagnostics, 20(3), 298-306.
Denning, D. W., O'driscoll, B. R., Hogaboam, C. M., Bowyer, P., & Niven, R. M. (2006). The link betweenfungi and severe asthma: a summary of the evidence. European Respiratory Journal, 27(3), 615-626.
Denning, D. W., Pashley, C., Hartl, D., Wardlaw, A., Godet, C., Del Giacco, S., & Sergejeva, S. (2014).Fungal allergy in asthma-state of the art and research needs. Clinical and translational allergy, 4, 1-23.
Donnelly, J.P., Chen, S.C., Kauffman, C.A., Steinbach, W.J., Baddley, J.W., Verweij, P.E., & Pappas, P.G.(2020). Revision and update of the consensus definitions of invasive fungal disease from the EuropeanOrganization for Research and Treatment of Cancer and the Mycoses Study Group Education and ResearchConsortium. Clinical Infectious Diseases, 71(6), 1367-1376.
Dumestre-Pérard, C., Lamy, B., Aldebert, D., Lemaire-Vieille, C., Grillot, R., Brion, J.P., & Cesbron, J.Y.(2008). Aspergillus conidia activate the complement by the mannan-binding lectin C2 bypass mechanism. TheJournal of Immunology, 181(10), 7100-7105.
Fayemiwo, S., Moore, C.B., Foden, P., Denning, D.W., & Richardson, M.D. (2017). Comparativeperformance of Aspergillus galactomannan ELISA and PCR in sputum from patients with ABPA and CPA.Journal of microbiological methods, 140, 32-39.
Felemban, H.S., Motahar, A.J., Alzamzami, N.M., Felemban, W.A., Adnan, A.M., Albishi, S.S., ... &Alzahrani, F.A. (2018). Causes and Management of Asthma. The Egyptian Journal of Hospital Medicine,70(1), 76-81.
Feshchenko, Y., Iashyna, L., Nugmanova, D., Gyrina, O., Polianska, M., Markov, A., ... & Vasylyev, A.(2017). Chronic obstructive pulmonary disease, bronchial asthma and allergic rhinitis in the adult populationwithin the commonwealth of independent states: rationale and design of the CORE study. Biology, Chemistryand pulmonary medicine Journal, 17(1), 1-8.
Foo, J., Landis, S.H., Maskell, J., Oh, Y.M., Van Der Molen, T., Han, M.K., ... & Punekar, Y. (2016).Continuing to confront COPD international patient survey: economic impact of COPD in 12 countries. PLOSone, 11(4), e0152618.
Fraczek, M.G., Kirwan, M.B., Moore, C.B., Morris, J., Denning, D.W., & Richardson, M.D. (2014). Volumedependency for culture of fungi from respiratory secretions and increased sensitivity of Aspergillusquantitative PCR. Mycoses, 57(2), 69-78.
Gaddeyya, G., Niharika, P.S., Bharathi, P., & Kumar, P.R. (2012). Isolation and identification of soilmycoflora in different crop fields at Salur Mandal Advances in Applied Science Research, 3(4), 2020-2026.
Gold, D.R., Adamkiewicz, G., Arshad, S.H., Celedón, J.C., Chapman, M.D., Chew, G.L., ... & Matsui, E.C.(2017). NIAID, NIEHS, NHLBI, and MCAN Workshop Report: the indoor environment and childhoodasthma-implications for home environmental intervention in asthma prevention and management. Journal ofAllergy and Clinical Immunology, 140(4), 933-949.
Hibbett, D.S., Binder, M., Bischoff, J.F., Blackwell, M., Cannon, P.F., Eriksson, O. E., ... & Zhang, N. (2007).A higher-level phylogenetic classification of the Fungi. Mycological research, 111(5), 509-547.
Hirose, K., Takahashi, K., & Nakajima, H. (2013). Roles of IL-22 in allergic airway inflammation. HindawiPublishing Corporation Journal of Allergy Volume 2013, 5/10.1155/2013/260518.
Holgate, S.T. (2011). Pathophysiology of asthma: what has our current understanding taught us about newtherapeutic approaches?. Journal of Allergy and Clinical Immunology, 128(3), 495-505.
Ishiguro, T., Takayanagi, N., Kagiyama, N., Shimizu, Y., Yanagisawa, T., & Sugita, Y. (2014). Clinicalcharacteristics of biopsy-proven allergic bronchopulmonary mycosis: variety in causative fungi and laboratoryfindings. Internal Medicine, 53(13), 1407-1411.
Kozel, T.R., & Wickes, B. (2014). Fungal diagnostics. Cold Spring Harbor perspectives in medicine, 4(4),a019299.
Kumar, R., Shrivastava, S.K., & Chakraborti, A. (2010). Comparison of broth dilution and disc diffusionmethod for the antifungal susceptibility testing of Aspergillus flavus. American Journal of BiomedicalSciences, 2(3), 202-208.
Latgé, J. P., & Chamilos, G. (2019). Aspergillus fumigatus and Aspergillosis in 2019. Clinical microbiologyreviews, 33(1), 10-1128.
Limper, A.H. (2010). The changing spectrum of fungal infections in pulmonary and critical care practice:clinical approach to diagnosis. Proceedings of the American thoracic society, 7(3), 163-168
Noori Ali, R., & Abdul Hussein S AL-Janabi, A. (2019). Asthma and Aspergillosis: Which one causes theother?. International Journal of Medical Reviews, 6(4), 140-145.
Nunes, C., Pereira, A. M., & Morais-Almeida, M. (2017). Asthma costs and social impact. Asthma researchand practice, 3(1), 1-11.
Postma, D.S. (2007). Gender differences in asthma development and progression. Gender medicine, 4, $133-S146.
Rick, E.M., Woolnough, K.F., Seear, P.J., Fairs, A., Satchwell, J., Richardson, Μ.. & Pashley, C.H. (2020).The airway fungal microbiome in asthma. Clinical & Experimental Allergy, 50(12), 1325-1341.
Rudramurthy, S. M., Jatana, M., Singh, R., & Chakrabarti, A. (2013). In vitro antifungal activity of Indianliposomal amphotericin B against clinical isolates of emerging species of yeast and moulds, and itscomparison with amphotericin B deoxycholate, voriconazole, itraconazole and fluconazole. Mycoses, 56(1),39-46.
Salehi, E., Hedayati, M.T., Zoll, J., Rafati, H., Ghasemi, M., Doroudinia, A., ... & Melchers, W.J. (2016).Discrimination of aspergillosis, mucormycosis, fusariosis, and scedosporiosis in formalin-fixed paraffin-embedded tissue specimens by use of multiple real-time quantitative PCR assays Journal of clinicalmicrobiology, 54(11), 2798-2803.
Salman, R. A., & Al-haddad, Z. A. (2021). Isolation and Identification of Aspergillus spp. from Human andSheep Respiratory Infection in Al-Qadisiyah Province. Systematic Reviews in Pharmacy, 12(3).
Tiwari, K.L., Jadhav, S.K., & Kumar, A. (2011). Morphological and molecular study of different Penicilliumspecies. Middle-East Journal Science Research, 7(2), 203-210.
Vergidis, P., Moore, C.B., Novak-Frazer, L., Rautemaa-Richardson, R., Walker, A., Denning, D.W., &Richardson, M.D. (2020). High-volume culture and quantitative real-time PCR for the detection ofAspergillus in sputum. Clinical Microbiology and Infection, 26(7), 935-940.
Wang, Z., Nilsson, R.H., James, T.Y., Dai, Y., & Townsend, J.P. (2016). Future perspectives and challengesof fungal systematics in the age of big data. Biology of Microfungi journal, 25-46.
Woodring, T., Deepe, G. S., Levitz, S. M., Wuethrich, M., & Klein, B. S. (2023, January). They shall notgrow mold: Soldiers of innate and adaptive immunity to fungi. In Seminars in immunology (Vol. 65, p.101673). NIH Public Access.
Yao, Y., Shi, L., Zhang, C., Sun, H., & Wu, L. (2019). Application of fungal fluorescent staining in oralcandidiasis: diagnostic analysis of 228 specimens. Biomedical Central microbiology, 19(1), 1-5.
Downloads
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Current Clinical and Medical Education