Femtosecond Lasers for Eye Surgery, Scanning Technology, Clinical Applications, Optical Coherence Tomography (OCT) and Alternative Imaging Technology
Keywords:
Femtosecond Lasers, Scanning Technology, Optical Coherence Tomography (OCT), Imaging TechnologyAbstract
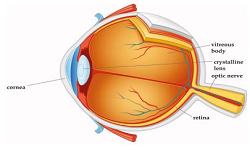
The field of ocular surgery has had a significant impact on medical laser
technology throughout the last four decades, and the reverse is also true. Because the eye,
cornea, lens, and vitreous body are optically transparent, it is much easier to deliver laser
energy at visible and near infrared (NIR) wavelengths at different focal depths through
these structures than through other types of tissue in the body. This allows for surgical
interventions to take place without opening or mechanically entering the eye, which is a
unique advantage of fs-Laser technology. Refractive corneal surgery, therapeutic cornea
treatments, and lens surgery were the original applications of fs-lasers. Additional novel
ophthalmic applications are also in the works. The most recent idea in laser systems is low
pulse energy and high pulse frequency. This allows for thermal tissue cutting with few side
effects since bigger numerical aperture focusing optics reduce the pulse energy needed for
optical breakdown. In the field of ophthalmic surgery, fs-laser technology has developed
into a highly accurate, dependable, and adaptable instrument during the last several
decades. Ergonomic and sturdy systems have become standard equipment in contemporary
operating theatres for eye surgery when coupled with ancillary technologies such as sterile
eye docking systems, optical coherence tomography (OCT) imaging, rapid laser scanning,
and sophisticated software. Global standards for fs-Laser-assisted cataract and corneal
surgery are now rather high.
Downloads
References
L. Zickler, M. Han, G. Giese, F. Loesel, J. Bille, Proceedings of The International Society for Optical Engineering (SPIE) 4978, 194–207 (2003) 3 Femtosecond Lasers in Ophthalmology 73 10. G. Mourou, Appl. Phys. B 65, 205–211 (1997)
CCME 2 (8), 344-362 (2024) VISION PUBLISHER|360
M. Kaschke, K.-H. Donnerhacke, and M. S. Rill, Optical Devices in Ophthalmology and Optometry: Technology, Design Principles and Clinical Applications, Weinheim, WILEY-VCH Verlag GmbH & Co. KGaA, 2014.
C. Latz, T. Asshauer, C. Rathjen, and A. Mirshahi, “Femtosecondlaser assisted surgery of the eye: overview and impact of the lowenergy concept,” Micromachines, vol. 12, no. 2, 2021.
R. Bhargava, P. Kumar, H. Phogat, and K. P. Chaudhary, “Neodymium-yttrium aluminium garnet laser capsulotomy energy levels for posterior capsule opacification,” J. Ophthalmic Vis. Res., vol. 10, no. 1, pp. 37–42, 2015.
A. Vogel, J. Noack, G. Hüttman, and G. Paltauf, “Mechanisms of femtosecond laser nanosurgery of cells and tissues,” Appl. Phys. B, vol. 81, no. 8, pp. 1015–1047, 2005.
A. Heisterkamp, T. Ripken, H. Lubatschowski, E. Lütkefels, W. Drommer, and W. Ertmer, “Intrastromal cutting effects in rabbit cornea using femtosecond laser pulses,” inOptical Biopsy and Tissue Optics, vol. 4161, Bellingham, SPIE, 2000, pp. 52–60.
A. Vogel, R. Busch, and U. Parlitz, “Shock wave emission and cavitation bubble generation by picosecond and nanosecond optical breakdown in water,” J. Acoust. Soc. Am., vol. 100, no. 1, pp. 148–165, 1996.
V. Venugopalan, “Mechanisms of pulsed laser ablation of biological tissues,” Chem. Rev., vol. 103, no. 2, pp. 577–644, 2003.
N. Tinne, G. Knoop, N. Kallweit, et al., “Effects of cavitation bubble interaction with temporally separated fs-laser pulses,” J. Biomed. Opt., vol. 19, no. 4, p. 048001, 2014.
H. Lubatschowski, G. Maatz, A. Heisterkamp, et al., “Application of ultrashort laser pulses for intrastromal refractive surgery,” Graefes Arch. Clin. Exp. Ophthalmol., vol. 238, no. 1, pp. 33–39, 2000
F. Loesel, J. Fischer, M.G¨otz, C. Horvarth, T. Juhasz, F. Noack, N. Suhm, J. Bille, Appl. Phys. B 66, 121–128 (1998)
F. Loesel, L. Zickler, R. Kessler, in Refractive Surgical Applications of Ultra short Pulse Lasers, ed by J. Bille, C. Harner, F. Loesel, New Frontiers in Vision and Aberration-Free Refractive Surgery, 1st ed.(Springer, Berlin Heidelberg New York, 2003), p. 159–175
T. Juhasz, F. Loesel, R. Kurtz, C. Horvath, J.F. Bille, G. Mourou, IEEE J. Quant. Electron. 5, 902–910 (1999)
Heisterkamp, T. Ripken, E. L¨utkefels, W. Drommer, H. Lubatschowski, W. Welling, W. Ertmer, Ophthalmologe 98, 623–628 (2001)
T. Juhasz, F. Loesel, C. Horvath, R. Kurtz, G. Mourou, Ultrafast Phenomena, 42–43 (1998) 16. M. Hamill, T. Kohnen, J. Cataract. Refract. Surg. 28, 328–336 (2002)
R. Kurtz, G. Spooner, K. Sletten, K. Yen, S. Sayegh, F. Loesel, C. Horvath, H. Liu, V. Elner, D. Cabrera, M.-H. Meunier, Z. Sacks, T. Juhasz, D. Miller, A. Williams, Proceedings of the SPIE 3616, 51–65 (1999)
W. Denk, J. Strickler, W. Webb, Science 248, 73–76 (1990) 20. W. Zipfel, R. Williams, W. Webb, Nat. Biotechnol. 21, 1369–1377 (2003)
B. Masters, Selected papers on multiphoton excitation microscopy, Milestone Series MS 175, (Bellingham, WA: SPIE Optical Engineering Press, 2003)
A. Yeh, N. Nassif, A. Zoumi, B. Tromberg, Opt. Lett. 27, 2082–2084 (2002) 23. M. Han, L. Zickler, G. Giese, M. Walter, J. Bille, Microscopic Evaluation of Femtosecond Laser Introstromal Surgery. Proceedings of The International Society for Optical Engineering (SPI), Munich 5142, 127–136 (2003)
J. Bille, C. Harner, F. Loesel, New Frontiers in Vision and Aberration-Free Refractive Surgery, 2nd edn. (Springer, Berlin Heidelberg New York, 2003)
CCME 2 (8), 344-362 (2024) VISION PUBLISHER|361
J. S. Pepose and H. Lubatschowski, “Comparing Femtosecond Lasers,” Cataract Refract. Surg. Today, pp. 45–51, 2008.
I. Ratkay-Traub, T. Juhasz, C. Horvath et al., “Ultra-short pulse (femtosecond) laser surgery: initial use inLASIK flap creation,” Ophthalmol. Clin. North Am., vol. 14, no. 2, pp. 347–355,
Z. Nagy and C. McAlinden, “Femtosecond laser cataract surgery,” Eye Vis., vol. 2, p. 11, 2015.
H. Lubatschowski, “Overview of commercially available femtosecond lasers in refractive surgery,” J. Refract.Surg., vol. 24, no. 1, pp. S102–S107, 2008.
A. K. Riau, Y. C. Liu, N. C. Lwin, et al., “Comparative study of nJand muJ-energy level femtosecond lasers:evaluation of flap adhesion strength, stromal bed quality, and tissue responses,” Invest. Ophthalmol. Vis. Sci.,vol. 55, no. 5, pp. 3186–3194, 2014.
W. J. Mayer, O. K. Klaproth, M. Ostovic, et al., “Cell death and ultrastructural morphology of femtosecondlaser-assisted anterior capsulotomy,” Investig. Ophthalmol. Vis. Sci., vol. 55, no. 2, pp. 893–898, 2014.
T. Schultz, S. C. Joachim, M. Stellbogen, and H. B. Dick, “Prostaglandin release during femtosecond laser-assisted cataract surgery: main inducer,” J. Refract. Surg., vol. 31, no. 2, pp. 78–81, 2015.
A. Vogel, “Energy balance of optical breakdown in water at ns to fs time scales,” Appl. Phys. B, vol. 68, no.2, pp. 271–280, 1999.
J. H. Talamo, P. Gooding, D. Angeley, et al., “Optical patient interface in femtosecond laser-assisted cataractsurgery: contact corneal applanation versus liquid immersion,” J. Cataract Refract. Surg., vol. 39, no. 4, pp.501–510, 2013.
A. F. Fercher, W. Drexler, C. K. Hitzenberger, and T. Lasser, “Optical coherence tomography – principles andapplications,” Rep. Prog. Phys., vol. 66, no. 2, pp. 239–303, 2003.
J. S. Schuman, C. A. Puliafito, J. G. Fujimoto, and J. S. Duker, Optical Coherence Tomography of OcularDiseases, New Jersey, Slack Inc., 2012.
A. F. Fercher, K. Mengedoht, and W. Werner, “Eye-length measurement by interferometry with partiallycoherent light,” Opt Lett., vol. 13, no. 3, pp. 1867–1869, 1988.
M. Wojtkowski, R. Leitgeb, A. Kowalczyk, T. Bajraszewski, and A. F. Fercher, “In vivo human retinalimaging by Fourier domain optical coherence tomography,” J. Biomed. Opt., vol. 7, no. 3, pp. 457–463, 2002.
O. Kermani, W. Fabian, and H. Lubatschowski, “Real-time optical coherence tomography-guidedfemtosecond laser sub-Bowman keratomileusis on human donor eyes,” Am. J. Ophthalmol., vol. 146, no. 1,pp. 42–45, 2008.
R. Ambrosio, Jr., B. F. Valbon, F. Faria-Correia, I. Ramos, and A. Luz, “Scheimpflug imaging for laserrefractive surgery,” Curr. Opin. Ophthalmol., vol. 24, no. 4, pp. 310–320, 2013.
M. Shajari, S. Khalil, G. Al-Khateeb, et al., “Comparison of 2 laser fragmentation patterns used infemtosecond laser-assisted cataract surgery,” J. Cataract Refract. Surg., vol. 43, no. 12, pp. 1571–1574, 2017.
D. S. Grewal, T. Schultz, S. Basti, and H. B. Dick, “Femtosecond laser-assisted cataract surgery–current statusand future directions,” Surv. Ophthalmol., vol. 61, no. 2, pp. 103–131, 2016.
D. Aron-Rosa, J. J. Aron, M. Griesemann, and R. Thyzel, “Use of the neodymium-YAG laser to open theposterior capsule after lens implant surgery: a preliminary report,” J. Am. Intraocul. Implant. Soc., vol. 6, no.4, pp. 352–354, 1980.
Z. Nagy, A. Takacs, T. Filkorn, and M. Sarayba, “Initial clinical evaluation of an intraocular femtosecondlaser in cataract surgery,” J. Refract. Surg., vol. 25, no. 12, pp. 1053–1060, 2009.
G. M. Kezirian and K. G. Stonecipher, “Comparison of the IntraLase femtosecond laser and mechanicalkeratomes for laser in situ keratomileusis,” J. Cataract Refract. Surg., vol. 30, no. 4, pp. 804–811, 2004.
CCME
Downloads
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Current Clinical and Medical Education