The Lifestyle of Pregnant Women and Its Impact on the Health of the Child after Birth TSB is a Model
Keywords:
Pregnant, Health of the Child, Birth TSBAbstract
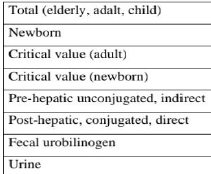
Worldwide, unconjugated hyperbilirubinemia still threatens the health of many newborn infants. Approximately 80% of term newborn infants develop physiologic unconjugated hyperbilirubinemia, which is transient and benign in the vast majority of these infants [1]. A small, but non-negligible proportion may develop severe neonatal hyperbilirubinemia (SNH). An estimated one million newborn infants worldwide suffer from SNH, necessitating intensive treatment to reduce the risk of death or kernicterus spectrum disorders (KSD) [2]. The incidence of SNH varies between 2 and 42 per 100,000 live-born infants in high-income countries (HIC) and depends, at least in part, on the predefined total serum bilirubin (TSB) concentration for this diagnosis
Downloads
References
Bhutani, V. K. et al. Predischarge screening for severe neonatal hyperbilirubinemia identifies infants who
need phototherapy. J. Pediatr. 162, 477-82. el (2013).
Bhutani, V. K. et al. Neonatal hyperbilirubinemia and Rhesus disease of the newborn: incidence and
impairment estimates for 2010 at regional and global levels. Pediatr. Res. 74, 86-100 (2013)
Donneborg, M.L., Hansen, B.M., Vandborg, P.K., Rodrigo-Domingo, M., Ebbesen, F. Extreme neonatal
hyperbilirubinemia and kernicterus spectrum disorder in Denmark during the years 2000-2015. J Perinatol. 40,
-202 (2020).
Greco, C. et al. Neonatal jaundice in low- and middle-income countries: lessons and future directions from the
Don Ostrow trieste yellow retreat. Neonatology 110, 172-80 (2016).
Bang, A. T., Bang, R. A., Baitule, S., Deshmukh, M. & Reddy, M. H. Burden of morbidities and the unmet
need for health care in rural neonates a prospective observational study in Gadchiroli, India. Indian Pediatr.
, 952- 65 (2001).
Ngashangva, L., Bachu, V. & Goswami, P. Development of new methods for determination of bilirubin. J.
Pharm. Biomed. Anal. 162, 272-85 (2019).
Hansen, T. W. R. Pioneers in the scientific study of neonatal jaundice and kernicterus. Pediatrics 106, e15
(2000).
CCME 2 (5), 125-133 (2024) VISION PUBLISHER|131
Kramer, L. I. Advancement of dermal Icterus in the jaundiced newborn. Am. J. Dis. Child 118, 454-8 (1969).
Davidson, L. T., Merritt, K. K. & Weech, A. A. Hyperbilirubinemia in the newborn. Am. J. Dis. Child 61,
-80 (1941).
Bhardwaj K, Locke T. Biringer A, Booth A, K Darling E, Dougan S, Harrison J, Hill S, Johnson A, Makin S,
Potter B. Newborn bilirubin screening for preventing severe hyperbilirubinemia and bilirubin encephalopathy:
a rapid review. Current Pediatric Reviews. 2017 Feb 1;13(1):67-90.
Meuwissen JA, Heirwegh KP. Aspects of bilirubin transport. InBilirubin 2018 Jan 18 (pp. 39-84). CRC Press.
Weaver L, Hamoud AR, Stec DE, Hinds Jr TD. Biliverdin reductase and bilirubin in hepatic disease.
American Journal of Physiology-Gastrointestinal and Liver Physiology. 2018 Jun 1;314(6):G668-76
Guerra Ruiz AR, Crespo J, López Martínez RM, Iruzubieta P, Casals Mercadal G, Lalana Garcés M, Lavin B,
Morales Ruiz M. Measurement and clinical usefulness of bilirubin in liver disease. Advances in Laboratory
Medicine/Avances en Medicina de Laboratorio. 2021 Aug 4:2(3):352-61.
Li D, Xia W, Cui X, Zhao M, Huang K, Wang X, Shen J, Chen H, Zhu L. The putatively high-altitude
adaptation of macaque monkeys: Evidence from the fecal metabolome and gut microbiome. Evolutionary
Applications. 2023 Oct;16(10):1708-20.
Yadav A, Yadav GA, Mala M. Diagnostic accuracy of transcutaneous bilirubinometer as non invasive method
to measure bilirubin in neonates.
Srinivas GL, Cuff CD, Ebeling MD, Mcelligott JT. Transcutaneous bilirubinometry is a reliably conservative
method of assessing neonatal jaundice. The Journal of Maternal-Fetal & Neonatal Medicine. 2016 Aug
:29(16):2635-9.
Phillips J, Henderson AC. Hemolytic anemia: evaluation and differential diagnosis. American family
physician. 2018 Sep 15;98(6):354-61.
Beris P, Picard V. Non-immune hemolysis: diagnostic considerations. InSeminars in hematology 2015 Oct 1
(Vol. 52, No. 4, pp. 287-303). WB Saunders.
Mendez SV. Correlation of Visual Assessment of Jaundice and Transcutaneous Bilirubin Levels with Serum
Bilirubin in Late Preterm and Term Neonates with Hyperbilirubinemia (Doctoral dissertation, Rajiv Gandhi
University of Health Sciences (India)).
Ansong-Assoku B, Shah S, Adnan M, Ankola P. Neonatal jaundice. StatPearls. 2024 Feb 12.#
Obeagu El, Katya MC. A Systematic Review on Physiological Jaundice: Diagnosis and Management of the
Affected Neonates. Madonna University journal of Medicine and Health Sciences ISSN: 2814-3035. 2022 Sep
;2(3):25-41.
Qian S, Kumar P, Testai FD. Bilirubin encephalopathy. Current Neurology and Neuroscience Reports. 2022
Jul;22(7):343-53
Olusanya BO, Kaplan M, Hansen TW. Neonatal hyperbilirubinaemia: a global perspective. The Lancet Child
& Adolescent Health. 2018 Aug 1;2(8):610-20.
Ullah S. Rahman K, Hedayati M. Hyperbilirubinemia in neonates: types, causes, clinical examinations,
preventive measures and treatments: a narrative review article. Iranian journal of public health. 2016
May;45(5):558.
Wagemann SC, Nannig PM. Severe hyperbilirubinemia in newborns, risk factors and neurological outcomes.
Rev. chil. pediatr. Santiago. 2019 Jun;90(3):267-74.
Muniyappa P. Kelley D. Hyperbilirubinemia in pediatrics: Evaluation and care. Current problems in pediatric
and adolescent health care. 2020 Aug 1:50(8):100842.
W. Wolkoff A, Berk PD. Bilirubin metabolism and jaundice. Schiff's Diseases of the Liver. 2017 Oct 25:103-
Abd El-Ghany SM, Monaem NA, El-Bagoury EM, Mohseb AI. THE IMPACT OF TYPE OF INFANT
FEEDING ON PHYSIOLOGICAL JAUNDICE IN EGYPTIAN ΝΕΟΝATES.
Cherepnalkovski AP, Krzelj V. Zafirovska-Ivanovska B, Gruev T, Markic J, Aluloska N, Zdraveska N.
Piperkovska K. Evaluation of neonatal hemolytic jaundice: clinical and laboratory parameters. Open Access
Macedonian Journal of Medical Sciences. 2015 Dec 12:3(4):694.
Sahoo T, Sahoo M, Gulla KM, Gupta M. Rh alloimmunisation: current updates in antenatal and postnatal
Management. The Indian Journal of Pediatrics. 2020 Dec:87:1018-28.
CCME 2 (5), 125-133 (2024) VISION PUBLISHER|132
Wickremasinghe AC, Kuzniewicz MW, McCulloch CE, Newman TB. Efficacy of subthreshold newborn
phototherapy during the birth hospitalization in preventing readmission for phototherapy. JAMA pediatrics.
Apr 1;172(4):378-85.
Agrawal A, Hussain KS, Kumar A. Minor blood group incompatibility due to blood groups other than Rh (D)
leading to hemolytic disease of fetus and newborn: a need for routine antibody screening during pregnancy.
Intractable & Rare Diseases Research. 2020 Feb 29:9(1):43-7.
Thakur AK, Ansari MA, Mishra A, Jha SK. Outcome of neonatal jaundice in term neonates with ABO
incompatibility at tertiary level center. International Journal of Contemporary Pediatrics. 2020
Oct;7(10):1973-7.
Chen HL, Wu SH, Hsu SH, Liou BY, Chen HL, Chang MH. Jaundice revisited: recent advances in the
diagnosis and treatment of inherited cholestatic liver diseases. Journal of biomedical science. 2018 Dec;25:1-
Wong RJ, Bhutani VK. Patient education: Jaundice in newborn infants (Beyond the Basics). UpToDate,
Available at: http://www. uptodate. com/contents/jaundice-in-newborn-infantsbeyond-the-basics (Accessed 5
September 2016). 2016.
Gazzin S, Masutti F, Vitek L. Tiribelli C. The molecular basis of jaundice: An old symptom revisited. Liver
International. 2017 Aug;37(8):1094-102.
Khan RS, Houlihan DD, Newsome PN. Investigation of jaundice. Medicine. 2015 Oct 1;43(10):573-6.
Abbas MW, Shamshad T, Ashraf MA, Javaid R. Jaundice: a basic review. Int J Res Med Sci. 2016
May;4(5):1313-9.
Abbas MW, Shamshad T, Ashraf MA, Javaid R. Jaundice: a basic review. Int J Res Med Sci. 2016
May;4(5):1313-9.
Gondal B, Aronsohn A. A systematic approach to patients with jaundice. InSeminars in interventional
radiology 2016 Dec (Vol. 33, No. 04, pp. 253- 258). Thieme Medical Publishers.
Bhardwaj K, Locke T, Biringer A, Booth A, K Darling E, Dougan S, Harrison J. Hill S, Johnson A, Makin S,
Potter B. Newborn bilirubin screeningfor preventing severe hyperbilirubinemia and bilirubin encephalopathy:
a rapid review. Current Pediatric Reviews. 2017 Feb 1;13(1):67-90.
Akangire G, Carter B. Birth injuries in neonates. Pediatrics in review. 2016 Nov 1;37(11):451-62.
Sriraman NK, Kellams A. Breastfeeding: What are the barriers? Why women struggle to achieve their goals.
Journal of women's health. 2016 Jul 1:25(7):714-22.
Gao C, Guo Y, Huang M, He J, Qiu X. Breast milk constituents and the development of breast milk jaundice
in neonates: A systematic review. Nutrients. 2023 May 10;15(10):2261.
Hossain M, Begum M, Ahmed S, Absar MN. Causes, management and immediate complications of
management of neonatal jaundice? A hospital- based study. Journal of Enam medical college. 2015
May:5(2):104-9.
Fargo MV, Grogan SP, Saguil A. Evaluation of jaundice in adults. American family physician. 2017 Feb
;95(3):164-8.
Pavlovic Markovic A, Stojkovic Lalosevic M, Mijac DD, Milovanovic T, Dragasevic S, Sokic Milutinovic A,
Krstic MN. Jaundice as a diagnostic and therapeutic problem: A general practitioner's approach. Digestive
Diseases. 2022 May 10:40(3):362-9.
Harsha L, Priya J, Shah KK, Reshmi B. Systemic approach to management of neonatal jaundice and
prevention of kernicterus. Research Journal of Pharmacy and Technology. 2015;8(8):1087-92.
Ahmadpour-kacho M, Zahed Pasha Y, Moghadamnia AA, Khafri S, Vafaeinezhad M. The effect of oral
fenofibrate on serum bilirubin level interm neonates with hyperbilirubinemia: a randomized clinical trail.
International Journal of Pediatrics. 2018 Oct 1;6(10):8317-27.
ALHARIS FM, ALBAKAA AA, NASRAWI AJ, SHUAIB AM. The role of Albumin infusion before
exchange transfusion in term neonates with hyperbilirubinemia. International Journal of Pharmaceutical
Research (09752366). 2020 Jul 1;12(3).
Zaghloul El Sayed D, Mohamed Said K, Mohamed Abdullah R. Improving Nurses' Performance Regarding
Care of Neonates with Hyperbilirubinemia Undergoing Blood Exchange: An Educational Program. Journal of
Nursing Science Benha University. 2024 Jan 1;5(1):572-83.
CCME 2 (5), 125-133 (2024) VISION PUBLISHER|133
Tewari D, Mocan A, Parvanov ED, Sah AN, Nabavi SM, Huminiecki L, Ma ZF, Lee YY, Horbańczuk JO,
Atanasov AG. Ethnopharmacological approaches for therapy of jaundice: Part I. Frontiers in pharmacology.
Aug 15:8:518.
Bassari R, Koea JB. Jaundice associated pruritis: a review of pathophysiology and treatment. World Journal of
Gastroenterology: WJG. 2015 Feb 2;21(5):1404.
Downloads
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Current Clinical and Medical Education